Breast infections are common, particularly among breastfeeding mothers. If left untreated, these infections can cause significant discomfort, pain, and distress.
In this article, we will explore the details of these infections, including their definitions, types, causes, and the importance of prompt treatment, including the use of antibiotics.
What are Breast Infections?
Breast infections, also known as mastitis, are inflammatory conditions that affect the breast tissue. They can be classified into two main categories:
- Mastitis: Inflammation of the breast tissue, often accompanied by infection.
- Abscesses: Pockets of pus that form in the breast tissue, typically as a result of untreated mastitis.
Common Causes of Breast Infections
Breast infections can arise from various factors, including:
- Weakened immune system
- Bacterial growth (usually Staphylococcus aureus)
- Clogged milk ducts (during breastfeeding)
- Skin lesions or cracks
- Poor hygiene

The Importance of Prompt Treatment
Prompt treatment of breast infections is crucial to prevent complications, such as:
- Abscess formation
- Septicemia (blood infection)
- Chronic pain
- Scarring
- Impact on breastfeeding (if applicable)
Recommended Readings:
- Antibiotics For Stomach Infection | Antibiotics For Gastroenteritis
- Best Antibiotics For Vaginal Infection | Vaginal Itching
- Antibiotics For UTI | Antibiotics For UTI In Men+Women
- Antibiotics For UTI | Antibiotics For UTI In Men+Women
Symptoms Of Breast Infections: Recognizing The Warning Signs

Table Of Contents
Common Symptoms Of Breast Infections
- Pain: Tenderness, aching, or sharp pain in the breast
- Redness: Erythema (redness) or discoloration of the breast skin
- Swelling: Enlargement or inflammation of the breast
- Warmth: Increased warmth or heat in the affected area
- Pus or discharge: Presence of pus or abnormal discharge from the nipple
- Fever: Elevated body temperature (usually above 100.4°F)
- Chills: Feeling cold, despite normal body temperature
- Fatigue: Feeling unusually tired or weak
- Swollen lymph nodes: Enlargement of lymph nodes in the armpit
When To Seek Medical Attention
Breast infections can manifest with a range of symptoms, which may vary in severity. It’s essential to be aware of these signs to seek medical attention promptly.

If you experience any of the following, seek medical attention immediately:
- Severe pain that doesn’t respond to pain relievers
- Increasing redness or swelling that spreads beyond the affected area
- Pus or discharge that’s thick, yellow, or foul-smelling
- Fever above 101.5°F (38.6°C)
- Chills or shaking
- Difficulty breastfeeding (if applicable)
- No improvement with self-care measures or antibiotics within 48-72 hours
Early recognition and treatment of breast infections can help prevent complications and promote effective management. In the next section, we’ll discuss the diagnosis and treatment options, including antibiotics.
Types Of Breast Infections: Understanding The Differences
Breast infections c Y7an be classified into three main categories: Mastitis, Breast Abscess, and Non-Lactational Infections. Each type has distinct characteristics, causes, and risk factors.
Mastitis
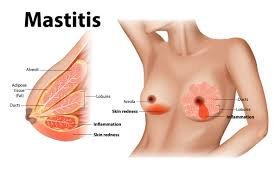
- Definition: Inflammation of the breast tissue, often accompanied by infection.
- Causes:
- Bacterial infection (usually Staphylococcus aureus)
- Breastfeeding (lactational mastitis)
- Clogged milk ducts
- Cracked or sore nipples
- Risk Factors:
- Poor breastfeeding technique
- Infrequent feeding or incomplete emptying of the breast
- Tight clothing or bras
- Previous history of mastitis
Breast Abscess

- Definition: A pocket of pus that forms in the breast tissue, usually as a result of untreated mastitis.
- Differences from Mastitis:
- The presence of a localized collection of pus
- Often more severe than mastitis
- May require surgical drainage
- Causes and Symptoms:
- Bacterial infection (usually Staphylococcus aureus)
- Untreated or severe mastitis
- Symptoms: severe pain, swelling, redness, warmth, and pus or discharge
Non-Lactational Breast Infections
- Definition: Breast infections unrelated to breastfeeding.
- Causes:
- Surgery (e.g., breast biopsy, implant placement)
- Trauma (e.g., breast injury)
- Immune system disorders (e.g., diabetes, HIV/AIDS)
- Bacterial or fungal infections
- Risk Factors:
- Weakened immune system
- Poor wound care or healing
- Pre-existing breast conditions (e.g., fibrocystic changes
Treatment Options For Breast Infections: A Comprehensive Approach
Effective treatment of these infections requires a combination of antibiotics, supportive care, and lifestyle modifications.
Overview of Treatment Strategies
- Antibiotics: Crucial for treating bacterial breast infections
- Supportive Treatments:
- Pain management (e.g., acetaminophen, ibuprofen)
- Rest and relaxation
- Warm compresses or breastfeeding support (if applicable)
- Proper wound care (if applicable)
Best Antibiotics for Breast Infections
- First-Line Antibiotics:
- Dicloxacillin: Effective against Staphylococcus aureus, commonly used for lactational mastitis
- Cephalexin: Broad-spectrum antibiotic, suitable for non-lactational breast infections
- Commonly Prescribed Antibiotics:
- Amoxicillin-Clavulanate: Broad-spectrum antibiotic, effective against various bacteria
- Clindamycin: Used for severe or recurrent infections, especially in cases of MRSA
- Dosage and Duration of Treatment:
- Typically 10-14 days, depending on the severity and type of infection
- Dosage varies based on the antibiotic and individual patient needs
Popular Antibiotics for Breast Infections
1. Amoxicillin
Is Amoxicillin Safe for Breast?
Amoxicillin is a commonly prescribed antibiotic for breast infections, particularly for lactating women. It is generally considered safe and effective in treating bacterial infections, including those affecting the breast tissue. However, it’s essential to consult a healthcare professional before taking amoxicillin, as they will determine the appropriate dosage and ensure it’s safe for you and your baby (if breastfeeding).
2. Ciprofloxacin
Can Ciprofloxacin Treat Breast Infection?
Ciprofloxacin is a broad-spectrum antibiotic that can treat various bacterial infections, including breast infections. However, it’s not typically the first choice for breast infections, especially in lactating women, due to its potential to pass into breast milk. Ciprofloxacin may be prescribed for more severe or resistant infections, but only under the guidance of a healthcare professional.
Topical Antibiotics and Creams
What Cream is Good for Breast Infection?
Topical antibiotics and creams can effectively treat mild to moderate breast infections, especially when combined with oral antibiotics.
Some popular options include:
| Cream/Topical Antibiotic | Effectiveness |
|---|---|
| Mupirocin (Bactroban) | Effective against Staphylococcus aureus and Streptococcus pyogenes |
| Neosporin | Broad-spectrum antibiotic cream for minor infections |
| Bacitracin | Effective against Staphylococcus aureus and Streptococcus pyogenes |
| Hydrocortisone cream | Reduces inflammation and swelling |
It’s crucial to consult a healthcare professional before using any topical antibiotics or creams to ensure proper diagnosis and treatment. They may prescribe a combination of oral and topical antibiotics for optimal results.
Important Considerations
- Antibiotic Resistance: Overuse or misuse of antibiotics can lead to resistance
- Allergic Reactions: Monitor for signs of allergic reactions, such as rash or difficulty breathing
- Breastfeeding Support: Continue breastfeeding, if possible, to help clear the infection and prevent further complications
Dosage And Administration
Dosage Guidelines for Mastitis Treatment
The dosage and duration of antibiotic therapy for mastitis treatment depend on the severity of the infection, the type of antibiotic prescribed, and individual patient factors.
Mastitis Treatment Antibiotics Dosage
| Antibiotic | Typical Dosage | Duration |
|---|---|---|
| Amoxicillin | 500-875 mg every 8-12 hours | 10-14 days |
| Ciprofloxacin | 500-750 mg every 12 hours | 10-14 days |
| Mupirocin (topical) | Apply 3-4 times a day | 7-10 days |
Duration Of Antibiotic Therapy
The typical duration of antibiotic therapy for mastitis is 10-14 days. However, your healthcare provider may adjust the duration based on your response to treatment.
Importance Of Completing The Full Course Of Antibiotics
It’s crucial to complete the full course of antibiotics as prescribed, even if symptoms improve before finishing the medication. This ensures that the infection is fully cleared and reduces the risk of antibiotic resistance.
What If Antibiotics Don’t Work?
Breast Infections Not Responding to Antibiotics
If your breast infection doesn’t respond to antibiotics, it’s essential to consult your healthcare provider for further evaluation.
Causes Of Treatment Failure
- Inadequate dosage or duration of antibiotic therapy
- Resistance to the prescribed antibiotic
- Presence of an abscess or other complications
- Underlying conditions, such as diabetes or immunodeficiency
Next Steps
- Further testing, such as imaging studies or cultures, to determine the cause of treatment failure
- Alternative treatments, such as drainage of an abscess or switching to a different antibiotic
- Referral to a specialist, such as a breast surgeon or infectious disease specialist, for further management
Home Remedies And Supportive Care: Enhancing Recovery
In addition to antibiotics, complementary treatments and supportive care can aid recovery and alleviate symptoms.
Complementary Treatments
- Warm Compresses: Apply a warm, damp washcloth to the affected area for 15-20 minutes, 3-4 times a day
- Proper Breastfeeding Techniques: For lactational infections, ensure proper latching, frequent feeding, and complete emptying of the breast
- Breast Massage: Gentle massage can help clear blocked ducts and promote milk flow
Pain Relief Options
- Over-the-counter Pain Relievers:
- Ibuprofen (e.g., Advil, Motrin)
- Acetaminophen (e.g., Tylenol)
- Topical Pain Relievers: Apply topical creams or ointments, such as arnica or capsaicin, to the affected area
Hydration and Rest
- Importance of Staying Hydrated: Drink plenty of water (at least 8-10 glasses a day) to help flush out toxins and support healing
- Getting Enough Rest: Aim for 8-10 hours of sleep per night to aid in recovery and immune function
Dietary Considerations
- Nutritional Support: Focus on whole, nutrient-rich foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats
- Increase Vitamin C Intake: Foods high in vitamin C (e.g., citrus fruits, leafy greens) can help boost the immune system
- Probiotics: Consider adding probiotic-rich foods (e.g., yogurt, kefir) or supplements to support gut health and immune function
Incorporating these home remedies and supportive care measures can enhance your recovery, alleviate symptoms, and promote overall well-being.
Prevention of Breast Infections: Empowering Yourself
Preventing breast infections requires a combination of knowledge, self-care, and proactive measures. By adopting these strategies, you can reduce the risk of developing breast infections.
Preventing Mastitis During Breastfeeding
- Proper Breastfeeding Techniques:
- Ensure proper latching and positioning
- Avoid over-tight clothing or bras
- Use breast pads or shields if needed
- Regular Feeding/Pumping:
- Frequent feeding (8-12 times in 24 hours)
- Regular pumping or expression (if unable to breastfeed)
- Recognizing Early Signs of Mastitis:
- Monitor for redness, swelling, pain, or fever
- Seek medical attention if symptoms persist or worsen
Prevention After Surgery or Trauma
- Proper Wound Care:
- Follow post-operative instructions
- Keep the wound clean and dry
- Monitor for signs of infection (redness, swelling, increased pain)
- Monitoring for Signs of Infection:
- Watch for increased redness, swelling, or pain
- Report any unusual symptoms to your healthcare provider
General Preventive Measures
- Maintaining Good Hygiene:
- Wash your hands frequently
- Clean and dry the breast area regularly
- Strengthening the Immune System:
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Stay hydrated and get enough sleep
- Manage stress through relaxation techniques (e.g., meditation, deep breathing)
By following these preventive measures, you can significantly reduce the risk of developing breast infections and promote overall breast health. Remember, early detection and treatment are crucial in preventing complications and ensuring effective management.
When to Consult a Doctor: Seeking Medical Attention
If you’re experiencing any of the following signs or symptoms, consult a doctor promptly:
Signs That Require Medical Attention
- Persistent Symptoms: If symptoms persist or worsen despite home treatment
- High Fever and Worsening Pain: Fever above 101.5°F (38.6°C) and increasing pain
- Presence of a Lump or Abscess: A palpable lump or abscess in the breast tissue
- Unusual Discharge: Abnormal discharge or pus from the nipple
- Changes in Breast Appearance: Changes in breast shape, size, or color
Possible Complications
- Delayed Treatment Risks: Untreated breast infections can lead to:
- Chronic mastitis or recurring infections
- Abscess formation or pocketing
- Scarring or fibrosis
- Increased risk of breast cancer (in rare cases)
- Chronic Mastitis: Recurring or persistent inflammation can lead to chronic mastitis
Consultation and Diagnosis
- Importance of a Professional Diagnosis: Accurate diagnosis is crucial for effective treatment and preventing complications
- Diagnostic Methods:
- Physical Exam: Visual inspection and palpation of the breast tissue
- Ultrasound: Imaging to detect abscesses or other abnormalities
- Culture Tests: Laboratory analysis of discharge or tissue samples to identify bacterial or fungal infections
- Biopsy: Tissue sampling for histopathological examination (if necessary)
Don’t hesitate to seek medical attention if you’re experiencing any unusual symptoms or signs. Early consultation and diagnosis can ensure prompt treatment and prevent potential complications.
Frequently Asked Questions (FAQs) – Antibiotic For Breast Infection
What is the best antibiotic for breast infection?
The best antibiotic for breast infection depends on the severity and type of infection, but common choices include Amoxicillin, Ciprofloxacin, and Mupirocin.
What is the antibiotic of choice for breast infection?
Amoxicillin is often the antibiotic of choice for breast infections, especially for lactating women.
Which antibiotic tablet for breast infection?
Amoxicillin tablets are commonly prescribed for breast infections.
Can antibiotics clear breast lumps?
Antibiotics may help clear breast lumps caused by infections, but not all breast lumps are caused by infections. Further evaluation by a healthcare provider is necessary.
How long does it take for antibiotics to work on breast infections?
Antibiotics typically start showing improvement within 2-3 days, but it’s essential to complete the full course of treatment.
Can I take antibiotics for breast infection while breastfeeding?
Yes, some antibiotics like Amoxicillin are safe for breastfeeding women, but consult your healthcare provider before taking any medication.
What if I miss a dose of antibiotics for a breast infection?
Take the missed dose as soon as you remember, but don’t double the dose. Consult your healthcare provider if you have concerns.
Can antibiotics prevent breast infections?
Antibiotics can’t prevent breast infections, but practicing good hygiene, proper breastfeeding techniques, and seeking medical attention at the first sign of infection can reduce the risk.
How to treat breast infections without antibiotics?
Mild breast infections may be treated with topical creams, warm compresses, and pain management, but antibiotics are often necessary for more severe infections.
Can breast infections recur after antibiotic treatment?
Yes, breast infections can recur if the underlying cause isn’t addressed or if the infection isn’t fully cleared. Practice preventive measures and seek medical attention if symptoms return.
What are the side effects of antibiotics for breast infections?
Common side effects include nausea, diarrhea, and allergic reactions. Consult your healthcare provider if you experience severe side effects.
Can I take pain relievers with antibiotics for breast infections?
Yes, pain relievers like acetaminophen or ibuprofen can be taken with antibiotics to manage pain and discomfort.
Can antibiotics treat fungal breast infections?
No, antibiotics are ineffective against fungal infections. Antifungal medications are necessary for fungal breast infections.
Can breast infections lead to sepsis?
Yes, untreated or severe breast infections can lead to sepsis, a life-threatening condition. Seek immediate medical attention if you experience severe symptoms.
Can antibiotics treat breast abscesses?
Antibiotics may be used in combination with drainage or surgical removal to treat breast abscesses.
How can I prevent breast infections while breastfeeding?
Practice good hygiene, proper latching, and frequent feeding to reduce the risk of breast infections.
Can I take antibiotics for breast infections during pregnancy?
Consult your healthcare provider before taking antibiotics during pregnancy, as some may not be safe for the developing fetus.
………………………….
Disclaimer:
Commissions we earn from partner links on this page do not influence our content. Our editorial content is based on thorough research and insights from qualified medical professionals to ensure the highest standards of accuracy and reliability.
Information provided on Doseway is for educational purposes only. Your health and wellness are unique to you, and the products and services we review may not be suitable for your individual circumstances. We do not offer personal medical advice, diagnosis, or treatment plans. For specific advice, please consult with a healthcare professional. Doseway adheres to strict editorial integrity standards. To the best of our knowledge, all content is accurate as of the date posted, though offers and information may change. The opinions expressed are the author’s own and have not been influenced, approved, or endorsed by our partners.

 Cart is empty
Cart is empty
Add a Comment